Nobody likes to think about observing their excrement after they’ve used the bathroom. However, being aware of what’s normal and what’s abnormal for you can serve as a valuable warning. You should especially notice when you have blood in your stools.
For some people, the blood may appear as a red tinge in the feces or the toilet. However, it can also be internal blood that makes your stools as dark as tar. You may also experience bright red smears on your bathroom tissue when cleaning yourself.
People are usually sensitive and embarrassed about talking about issues that deal with their colon or bowel movements. The Canadian Society of Intestinal Research states that it’s normal for people to have up to three bowel movements a day. However, some people are okay with three times a week, per the article.
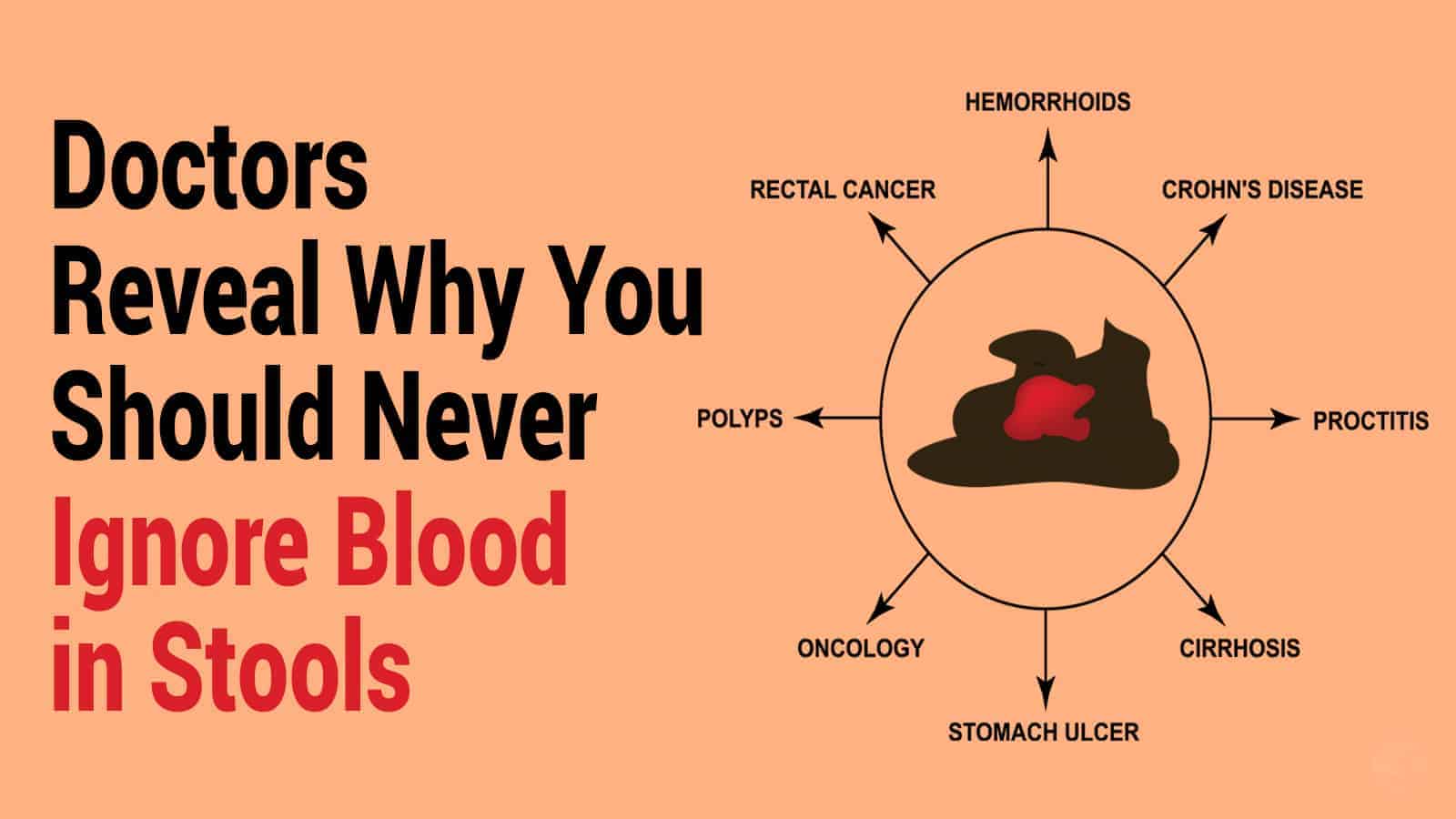
Gastrointestinal Conditions That May Cause Blood in Your Stool
 If you notice blood in your stool or on your bathroom tissue, you shouldn’t ignore it. Your body is giving you a warning that you should heed. Here are some common gastrointestinal conditions that may cause you to have blood in your stools.
If you notice blood in your stool or on your bathroom tissue, you shouldn’t ignore it. Your body is giving you a warning that you should heed. Here are some common gastrointestinal conditions that may cause you to have blood in your stools.
1. Hemorrhoids
According to an article from the US Library of Medicine, you can experience bleeding from your bowels when your rectum or anal veins become inflamed. Hemorrhoids can be either external or internal. If you have a sedentary job that requires a lot of sitting, you may be a prime candidate for the condition.
People who battle chronic constipation can strain too much while passing stools, affecting veins in the anus and rectum. It’s also common for expectant mothers to have excess pressure on their rectal veins, resulting in hemorrhoids. Blood in your stools from hemorrhoids is usually bright red, and you may notice it in the feces or on the bathroom tissue.
The condition often causes itching and painful swelling that makes sitting or going to the bathroom difficult. Hemorrhoids are often more of a bother than an extreme medical issue. However, abnormal bleeding or severe pain may require medical attention. Some people need surgery to remove painful hemorrhoids.
2. Anal Fissures
If you have bowel problems, the skin around your anal area is delicately thin and sensitive, says an article published by The National Center for Biotechnology Information. For these reasons, anal tears (also called fissures) are common for both children and adults. The article explains that these superficial tears develop around the anus due to chronic constipation or an acute accident.
Anal fissures are among the most common reasons for emergency room visits because of bleeding or blood in your stools. Fortunately, this condition can be treated with medical management. Sometimes, more serious tears may require surgery.
3. Peptic Ulcers
Did you know that ulcers can cause blood in your stools? A study published by the National Library of Medicine states that at least 5 million people in America have been diagnosed with peptic ulcers. An overload of digestive acids can eat away holes in the lining of the stomach or small intestines, resulting in this diagnosis.
Not everyone with peptic ulcers is symptomatic. However, most patients can experience stomach pain, bloating, nausea, or vomiting. Another common symptom is dark, tar-like blood in your stools.
Internal bleeding from peptic ulcers can cause anemia, and it can lead to a life-threatening loss of blood without medical intervention.
4. Diverticulitis
Experts aren’t sure what causes diverticulitis, which is an inflammatory condition of the colon. An article published by the National Institute of Diabetes, Digestive and Kidney Diseases explains this condition as small sacs protruding from weak spots in the colon wall. When these become inflamed, it becomes diverticulitis.
While the article says that most diverticulitis patients are asymptomatic, others experience severe abdominal pain, diarrhea, and constipation. The condition can cause blood to enter the bowels, causing the stool to be dark red in appearance. In these rare instances, patients may require surgery.
5. Gastroenteritis
Have you ever experienced an episode of painful gastroenteritis? It’s what people mistakenly call the “stomach flu.” In an article published by the National Institute of Diabetes and Digestive and Kidney Diseases, experts explain that gastroenteritis is caused by a virus attacking your intestines. Therefore, it technically involves the intestines and not your stomach.
However, it can cause acute symptoms like abdominal pain, nausea, vomiting, and watery stools. Gastroenteritis is caused by norovirus and is a common condition. In fact, according to the report, it affects about 21 million people each year.
Gastroenteritis may also cause acute blood in your stools. If you have flu-like symptoms and notice bloody clumps in your feces, you should immediately get medical attention. The medical staff can rule out other disorders that may be causing your bleeding.
6. Irritable Bowel Syndrome
Have you been diagnosed with irritable bowel syndrome? The International Foundation for Gastrointestinal Disorders defines IBS as occasional abdominal pain associated with diarrhea, constipation, or all three. While the disorder’s cause is still undetermined, the article mentions that some experts believe it could be genetics, infection, or trauma-related.
IBS often causes constipation, which can cause straining and blood in your feces. It’s an alarming symptom that you should report immediately to your healthcare specialist. Everybody is different, so it’s best not to take chances on your health.
 7. Ulcerative Colitis
7. Ulcerative Colitis
Another condition that may cause blood in your feces is ulcerative colitis. According to an article from Crohn’s & Colitis Foundation, ulcerative colitis is an autoimmune disease that causes your colon to become inflamed. The result of chronic inflammation is small ulcers throughout the lining of your large intestines.
Some of the ulcerative colitis symptoms include abdominal pain, diarrhea, and possibly blood in the stool. When you have open sores (ulcers) in your colon, it’s understandable that they can become irritated and bleed.
8. Colorectal Cancer
Do you have periodic screening for colorectal cancer? The American Cancer Society provides annual statistics for the disease. Current figures from the organization say that at least 104,610 new colon cancer cases were reported this year in the United States. Also, 43,340 new cases of rectal cancer were reported.
The good news from the statistics is that these numbers have dropped since the 1980s because of early screening/detection and lifestyle changes. Many patients report symptoms like a change in bowel habits, abdominal pain, bright red rectal bleeding, and dark brown or black stools.
9. Gastrointestinal Bleeding
The National Institute of Diabetes, Digestion, and Kidney Diseases defines gastrointestinal bleeding as losing blood anywhere in your digestive tract. The article says that it’s a symptom of another disease and isn’t categorized as a disease itself. You can be bleeding from your upper digestive tract (upper GI) or lower part (lower GI), explains the source.
One of the tell-tale symptoms of gastrointestinal bleeding is dark, tarry stools. Patients may also experience abdominal cramps, exhaustion, dizziness, and bright red blood in their vomit. The article also explains the dangers of occult bleeding, or hidden blood in the stools that only a lab test can detect.
10. Polyps
Polyps are small growths usually found in the large intestines and colon. They are of particular concern when you have a colonoscopy screening for colorectal cancer. A study published by the American Gastroenterological Association states that it’s common for small rectal polyps to cause minor bleeding. While the article says that younger patients with no colorectal cancer history usually have benign polyps, they still merit an examination.
Larger polyps are usually of more concern as they carry a more significant chance of being malignant. Routine examinations are essential to keep polyps removed and any further issues under control.
How Often Do You Need a Colorectal Screening?
The American Cancer Society has guidelines for when and how often you should have a colorectal screening. The agency suggests that screening should start at the age of 45 if your risks are of an average level. Normal risks include not having a personal or family history of cancerous polyps or colorectal cancer.
They recommend that you have a stool sample test annually to check for occult bleeding. It would be best if you had a colonoscopy every ten years. If you have a personal or family history of colorectal cancer, the screening guidelines vary according to your case.
However, you mustn’t avoid these tests simply because of the inconvenience, as they have saved many lives. Additionally, severe bleeds from the inside can also be detected on many blood tests, specifically ferritin levels.
 Final Thoughts about Blood in Your Stools
Final Thoughts about Blood in Your Stools
While it may be normal for some conditions to cause blood in your stool, it’s important not to ignore it. The bloody feces may be a sign of an underlying issue that can be serious. If you notice any signs of this type of bleeding, consult your primary healthcare provider as soon as possible.