Engineers and medical researchers at the University of Minnesota Twin Cities have found a new way to fight cancer. A groundbreaking study reveals how revolutionary cancer therapies using engineered immune cells boost a patient’s immune system. In turn, this gives the patient a better chance to fight cancer.
This research could lead to improved cancer therapies for millions of people. The study was published in the journal Nature Communications on May 14, 2021.
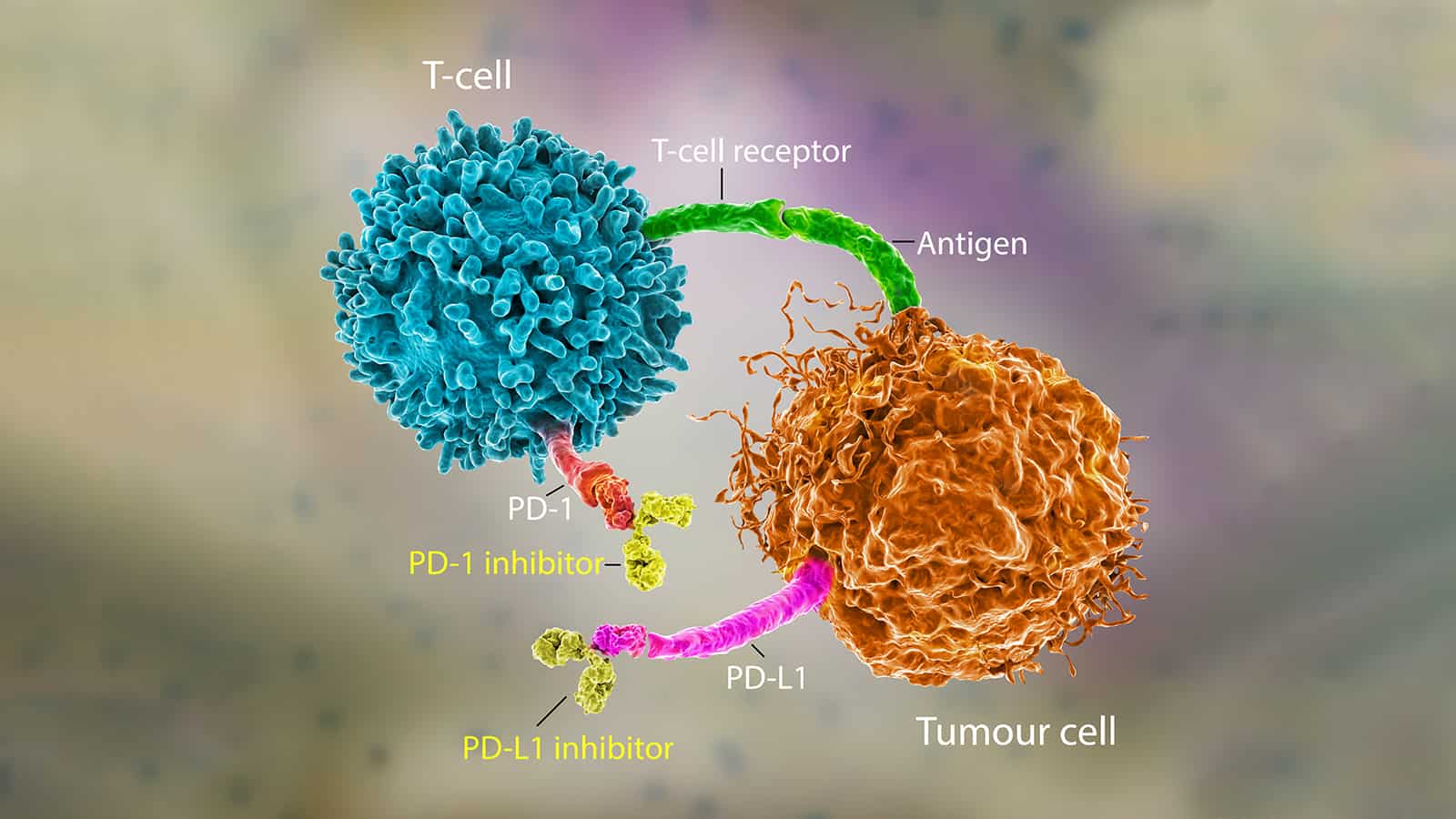
The new method of stimulating immune cells to fight cancer will make immunotherapy even more effective. Instead of using harmful chemicals or radiation, immunotherapy harnesses the patient’s immune system to prevent or eliminate cancer. The cancer treatment involves using T cells, a white blood cell playing a crucial role in immune responses to cancer. Scientists compare Cytotoxic T cells to soldiers because they seek out and destroy targeted cancer cells.
Many clinics use immunotherapy to treat various forms of cancer in the blood or blood-producing organs. It’s been widely successful, but T cells have a more challenging time destroying cancer cells in solid tumors.
Paolo Provenzano, the senior author of the study and a biomedical engineering associate professor at the University of Minnesota College of Science and Engineering, says the following:
“The tumor is sort of like an obstacle course, and the T cell has to run the gauntlet to reach the cancer cells. These T cells get into tumors, but they just can’t move around well, and they can’t go where they need to go before they run out of gas and are exhausted.”
 In this groundbreaking study, the researchers have worked on engineering the T cells to fight cancer more effectively. They’ve developed engineering design criteria that mechanically improve the cells to make them more capable of overcoming physical barriers. By enhancing the immune cells’ ability to recognize and find cancer cells, they have a higher probability of destroying the tumor.
In this groundbreaking study, the researchers have worked on engineering the T cells to fight cancer more effectively. They’ve developed engineering design criteria that mechanically improve the cells to make them more capable of overcoming physical barriers. By enhancing the immune cells’ ability to recognize and find cancer cells, they have a higher probability of destroying the tumor.
The study that engineers immune cells to fight cancer
Within fibrous masses of tumors, immune cells immediately slow down about two-fold due to the stiff nature of tumors. However, this new form of immunotherapy could help T cells maintain speed even in solid tumors.
“This study is our first publication where we have identified some structural and signaling elements where we can tune these T cells to make them more effective cancer fighters,” said Provenzano.
“Every ‘obstacle course’ within a tumor is slightly different, but there are some similarities. After engineering these immune cells, we found that they moved through the tumor almost twice as fast no matter what obstacles were in their way.”
To stimulate the cytotoxic T cells, authors utilized advanced gene-editing technologies, or genome editing, to alter DNA in the T cells. This way, the cells have a better chance of overcoming physical barriers within the tumor. Of course, immunotherapy aims to slow down or prevent the growth of cancer cells while speeding up immune cells.
The researchers have been working on engineering cells that can overcome various physical barriers. By combining these cells, the researchers hope the groups of immune cells can effectively overcome 100% of the obstacles to fight cancer cells.
Provenzano said they would keep analyzing the mechanical properties of the cells to gain more insight into how the immune cells and cancer cells interact. Currently, the team is studying engineered immune cells in rodents and will perform clinical trials in humans in the future. They’ve focused much of their initial research on pancreatic cancer. However, Provenzano said the methods could treat other cancers as well.
Engineering T cells to fight cancer is relatively new, but it has a bright future.
“Using a cell engineering approach to fight cancer is a relatively new field,” Provenzano said. “It allows for a very personalized approach with applications for a wide array of cancers. We feel we are expanding a new line of research to look at how our bodies can fight cancer. This could have a big impact in the future.”
The treatment utilizes the body’s T cells by either isolating the cells that already target tumors or genetically modifying the cells. Scientists then take these receptors (either natural T-cell receptors (TCRs) or synthetic receptors known as chimeric antigen receptors (CARs)), expand them, and reinfuse them into the patient.
The T cells that perform the best have been engineered to express CARs that target CD19. This pan-B-cell marker exists on most cancerous B cells. Thus far, many clinical trials found that 90% of advanced B-cell leukemia patients treated with CD19 CAR-T cells achieved total remission. This shows promise for the future of engineering immune cells to fight cancer.
In recent years, scientists made considerable breakthroughs in this exciting new way to treat cancer. In July 2017, the FDA Oncologic Drugs Advisory Committee approved the first product to treat B-cell acute lymphoblastic leukemia. The first CD19 CAR-T cell product, CTL019 (tisagenlecleucel) from Novartis, can treat cancer in pediatric and young adult patients.
Several other companies have been working to develop products that involve engineering T cells to fight cancer. Commercializing T-cell therapy will allow engineers to use their knowledge to expand the market for cellular products.
In the future, perhaps cancer won’t be as prevalent due to these groundbreaking forms of cancer therapy.
 Final thoughts on research showing how to stimulate immune cells to fight cancer
Final thoughts on research showing how to stimulate immune cells to fight cancer
A new study by researchers at the University of Minnesota reveals a revolutionary method of engineering immune cells to fight cancer. The team discovered that our bodies’ cells could destroy cancer, especially if they’ve been engineered to do so. There are still many unknowns regarding this form of therapy, but it shows promise. In fact, the FDA already approved one product that treats a type of leukemia using chimeric antigen receptors.
The latest research by the team from Minnesota could lead to even more treatments to fight cancer in the future.