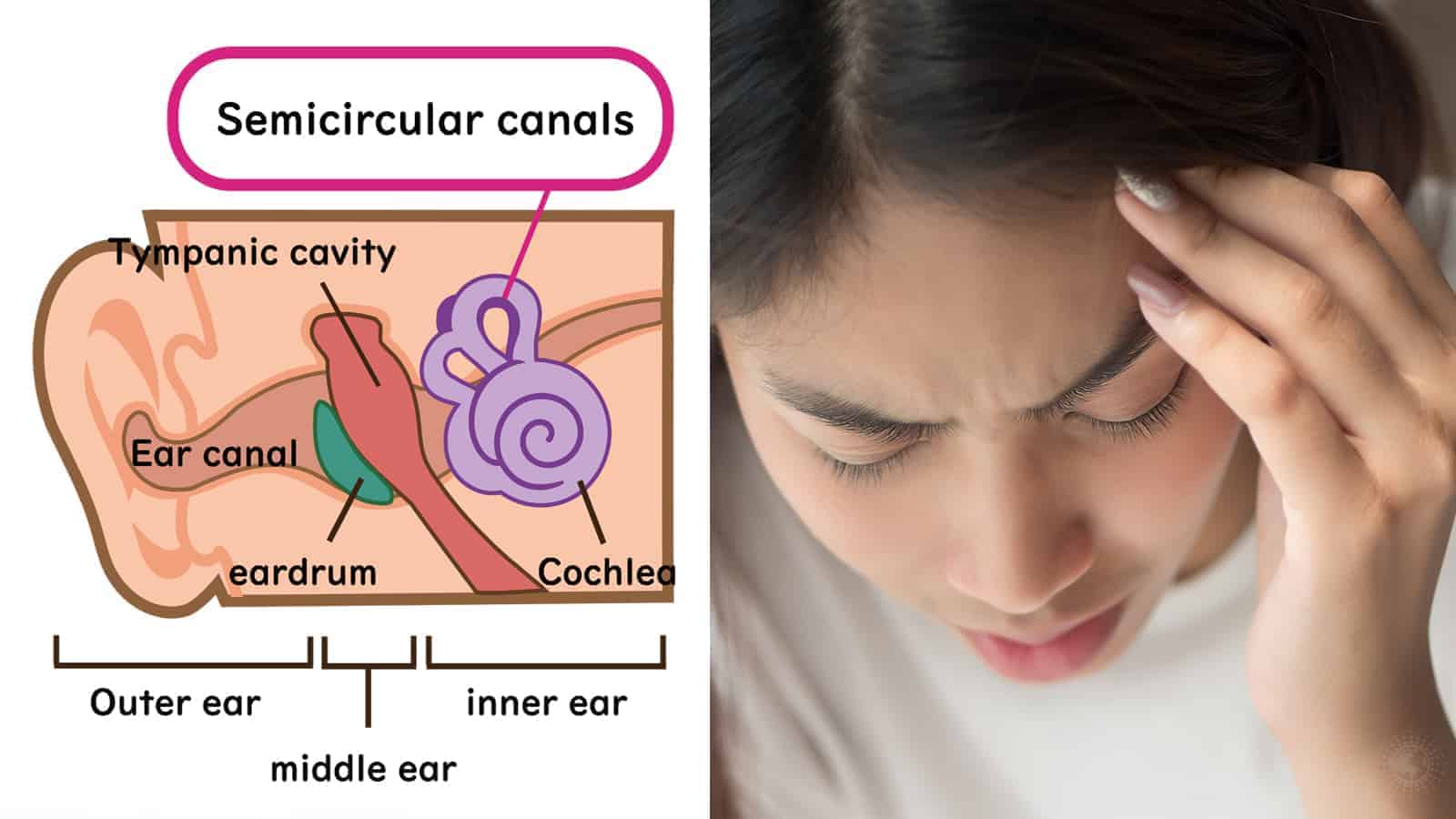
Ménière’s disease affects the inner ear, which is the part that is related to hearing and balance. It can be debilitating, uncomfortable, and frustrating to deal with each day.
It is an uncommon disorder typically diagnosed between the ages of 40 and 60 but can occur at any age. Treatment can help relieve the symptoms and minimize the impact on your life. Ménière’s caused unexpected attacks that can last for hours or days before the symptoms disappear.
It leads to dizzy spells and hearing loss, and it typically only affects one ear. This disorder also causes a roaring sound in your ears called tinnitus and the sensation of ear pressure or pain. Without treatment, this disease can lead to permanent hearing loss.
What is Ménière’s Disease?
Ménière’s disease is still being studied, but researchers discovered it develops from a pressure deep inside the ear. The pressure comes from fluid build-up within the ear.
Studies from the National Institute of Deafness and Other Communication Disorders show that nearly 615,000 people have Ménière’s disease and that cases are increasing. There is no cure, but you can do things to treat it while alleviating the symptoms. If you find a treatment option that works for you, remission is possible.
 What Causes Ménière’s Disease?
What Causes Ménière’s Disease?
If you have a family history of the disease, you are more likely to develop it yourself. Not everyone that is diagnosed has a genetic disposition, though. If the inner ear is damaged or the fluid levels are off, it can trigger Ménière’s.
Another trigger of this disease is chronic migraine headaches because they constrict the blood vessels. Sometimes, a blockage can lead to improper fluid drainage, which can cause Ménière’s to set in. Other causes include an abnormal immune response, allergies, or a viral infection.
Anytime fluid builds up in the inner ear, it stimulates sensory cells that signal the brain. Each time it sends a signal, you experience the symptoms of Ménière’s. Other potential causes of Ménière’s include:
- head injury
- alcohol use
- stress or anxiety
- medication side effects
- smoking
- fatigue
- respiratory infection
What Are the Symptoms of Ménière’s Disease?
The symptoms of this disease vary widely in each case. Some people might experience many symptoms, while others only experience one or two. Either way, knowing the signs can help you identify the disease.
The symptoms of Ménière’s disease include the following:
- Dizziness Or Lightheadedness: You will sometimes feel dizzy or lightheaded as a result of Ménière’s, making it dangerous to drive. When this happens to you, try to sit or lie down until the feeling passes.
- Pressure or a Feeling of Fullness in the Ear: If you experience a feeling of fullness or pressure in your ear, it is a sign of Ménière’s. This feeling will only occur in the affected ear.
- Tinnitus: Tinnitus is a ringing, buzzing, roaring, whistling, or hissing sound occurring in your ear.
- Hearing Loss: In Ménière’s, hearing loss might come and go, especially in the early stages. However, without treatment, the hearing loss can become permanent. People with Ménière’s tend to have problems hearing low frequencies or frequencies combined with low and high.
- Feeling Uneasy: If you feel uneasy or unstable, especially when in a darkened area, it is a sign of Ménière’s.
- Intense, Reoccurring Episodes of Vertigo: Vertigo is a spontaneous spinning sensation that starts and stops suddenly, and it sometimes causes nausea. You usually won’t get a warning, and each episode can last anywhere from 20 minutes to several hours, but no more than 24 hours.
- Blurred Vision and Eye Twitches: As Ménière’s worsens, your symptoms will intensify and change. After dealing with occasional bouts of vertigo for an extended time, you could develop vision and eye problems.
- Nausea Or Vomiting: This disease can cause nausea or vomiting as it affects your balance. It will make you feel sick, and the symptom worsens the more you move.
- Diplacusis: In some cases of Ménière’s, people experience diplacusis or double hearing.
- Fatigue: Attacks can last up to 24 hours, so they take quite a bit of energy out of you. Once the episode passes, you will likely feel an overwhelming need to rest.
Stages Of Ménière’s Disease
Ménière’s has been divided into multiple stages, making it easier to describe the condition. All of the phases differ, so understanding them can give you a better idea.
- Early Stage: During the early stage of Ménière’s, you might experience vertigo, tinnitus, lightheadedness, nausea, and vomiting. The severity of attacks during this phase varies, but they last anywhere from 20 minutes to a full day. A person might also experience a blocked or full ear and hearing loss during this stage.
- Middle Stage: The symptoms of vertigo, hearing loss, and tinnitus become more severe during the middle stage of Ménière’s. During this phase, people might also experience long-term remission that can last for up to several months.
- Late Stage: The late stage of Ménière’s involves less vertigo, and they might not experience it at all. Tinnitus and hearing loss get progressively worse during this phase, however. The person might suffer from unsteady balance regularly, and they’ll feel unstable in dark lighting conditions.
How Is Ménière’s Disease Diagnosed?
Experts explain that getting an official diagnosis for Ménière’s can be difficult and often takes several months to attain. The reason it is so hard is that doctors must rule out other diseases with similar symptoms first. Some of the diagnostic methods the doctor might use include:
- Physical Exam and Review of Your Medical History: Your doctor will want to know how many episodes of vertigo you experienced and the duration of each. They will ask about episodes of tinnitus or fullness in your ear. Your doctor will also do a physical assessment to check for other causes of Ménière’s disease symptoms.
- Hearing Assessment: For a Ménière’s diagnosis, your doctor will do a hearing test or audiometry. This test assesses your ability to detect sound at different pitches and volumes, and it will determine how well you can distinguish between similar-sounded words.
- Balance Assessment: When you have Ménière’s, you might experience balance issues that return to normal between episodes. Other times, you might have ongoing balance problems. There are several tests that your doctor might do to evaluate your balance.
- Tests to Rule Out Other Conditions: Your doctor might request blood tests and imaging scans to rule out other disorders with similar symptoms. Once they begin to rule out other conditions, the diagnosis process becomes easier.
 How Is Ménière’s Disease Treated?
How Is Ménière’s Disease Treated?
Doctors will suggest treatment options to you to help manage the symptoms and alleviate the issues that accompany Ménière’s. While there is no cure, treating the symptoms can help you enter remission. Some of the ways that Ménière’s disease is treated include:
- Try Medication: Doctors sometimes prescribe medications to control the symptoms of Ménière’s. Studies show that with medication, your chances of controlling the condition increase by about 80%.
- Take Water Pills: Water pills help reduce the sodium levels in your body but have unpleasant side effects. However, the reduced sodium will help limit the frequency and severity of your attacks.
- Vestibular Rehabilitation Therapy: This therapy can help retrain your brain to process balance differently. If balance issues are making your life hard, vestibular rehabilitation therapy can make a difference.
- Surgery: Your doctor will save surgery for the last option because it is the most invasive. One of the surgeries they might suggest will relieve excessive pressure from the inner ear. The other type your doctor will consider is surgery to stop the signals from your ear to your brain.
- Hearing Aid: If you’ve experienced hearing loss due to Ménière’s, a hearing aid can help. Not only will it improve your hearing, but you’ll feel better and more stable, too.
- Middle Ear Injections: Your doctor might suggest injecting medication into the middle ear. The medications will absorb into the inner ear, improving vertigo symptoms.
Lifestyle Changes for Ménière’s Disease
- There are things you can change about your life to help with Ménière’s disease, including:
- Changing Your Diet: Your diet can help manage the symptoms of this disease, so acknowledging the foods you ate before an attack can help. Keep a journal to see which foods seem to trigger it, and try to eliminate them from your diet. One of the biggest dietary issues for Ménière’s is sodium, so reduce your intake as much as you can.
- Avoid Things That Worsen Vertigo: Anytime you experience vertigo, avoid sudden movements, bright lights, looking at electronics screens, or reading. If you can, sit or lie down when you feel dizzy and stay in that position until it passes. It might help to look at something that isn’t moving, too.
- Limit Caffeine, Alcohol, and Tobacco: Caffeine, alcohol, and tobacco are three substances that can negatively affect the fluid balance in your ears. It can trigger Ménière’s episodes and worsen the symptoms.
- Work on Stress Management: Stress and anxiety are both causes and symptoms of Ménière’s disease. If you can learn how to manage stress, you will experience an improvement in your condition.
What Is the Outlook for Someone with Ménière’s Disease?
More than half of the people that suffer from Ménière’s disease get better without help. They can control their symptoms with a change in their diet or with help from a doctor.
With hearing loss, you might develop fear or a loss of confidence. You might also experience anxiety about a conversation with others, causing depression.
There is no cure for Ménière’s, but you can alleviate the symptoms and complications. Plus, with the right treatment methods, you can enter remission.
 Final Thoughts on Meniere’s Disease: Symptoms, Causes, Diagnosis, and Treatment
Final Thoughts on Meniere’s Disease: Symptoms, Causes, Diagnosis, and Treatment
Living with Ménière’s syndrome is difficult, but you can manage the symptoms and alleviate the severity. This disease affects your ability to walk, hear, and live a normal life. While it isn’t curable, you can manage it and aim for remission.
Talk to your doctor for a diagnosis and treatment options, and make lifestyle changes to help yourself at home. If you can get ahead of worsening conditions, you can avoid the more invasive treatment options and symptoms.