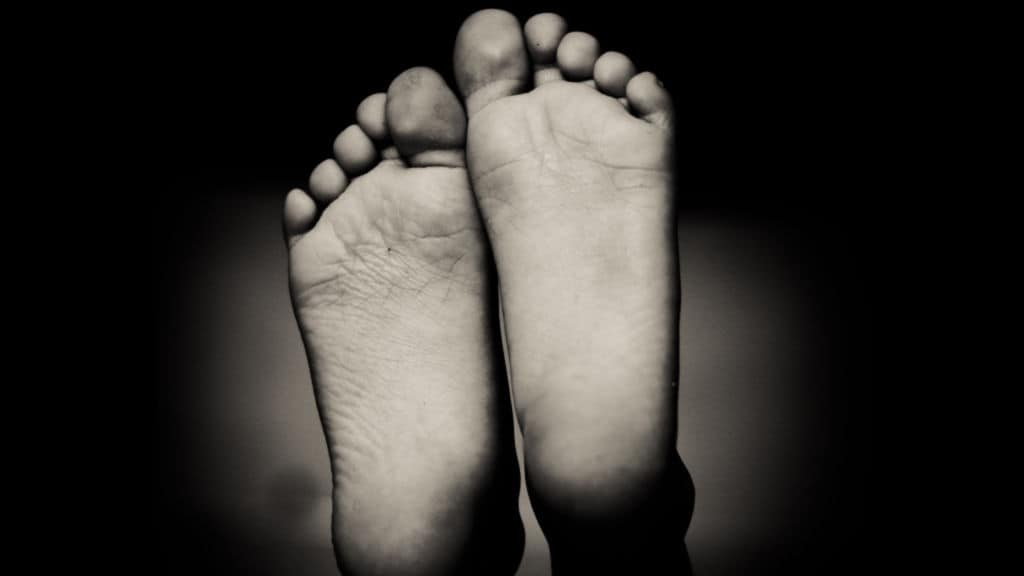
Plantar fasciitis is a widespread cause of heel pain. Patients typically experience a stabbing pain in the sole of their foot around the heel. The condition may (or may not) be accompanied by a heel spur.
The pain is usually at its worst first thing in the morning, but it gradually decreases after the patient starts walking. Similarly, the condition becomes increasingly painful if the patient has been standing for a long time, or if they get up after a long period of sitting. The pain also becomes more acute after exercise rather than during it.
What Causes Plantar Fasciitis?
Plantar fasciitis usually manifests as an inflammation of the plantar fascia, which is a thick band of tissue, which is shaped like a bowstring, running across the sole. It connects the heel bone to the toes. The plantar fascia acts as a shock absorber and supports the arch of the foot.
If too much stress wears on the plantar fascia, it can develop small tears. Eventually, those tears cause the plantar fascia to become inflamed and irritated. Determining the causes of those tears can be difficult as it is generally not clear-cut. The patient is usually not able to point to a specific event, like a fall, that caused their condition.
Possible Causes
The condition arises typically from an inflammation of the plantar fascia. However, researchers argued in a 2003 paper that degeneration of the plantar fascia caused it. In the “Journal of the American Podiatric Medical Association,” scientists studied 50 cases in which patients underwent heel spur surgery. They found signs of degeneration rather than inflammation and thus argued that the condition should earn the new name “plantar fasciosis.”
In 2019, StatPearls, an online medical journal, published a description of the condition that called it “the result of degenerative irritation.” It seemed to agree with the 2003 paper that it was not a type of inflammation since doctors generally don’t find inflammatory cells during diagnosis. Instead, it is an injury that is often caused by overuse in which repeated pressure or strain causes the plantar fascia to develop tiny tears. About half the patients will also have at least one heel spur, but a heel spur does not irritate the plantar fascia.
What’s a heel spur?
A heel spur, if you’re wondering, is a bony growth called a calcium deposit that usually develops under the front part of the heel. While some heel spurs are virtually undetectable by the naked eye, others can grow to half an inch in length. A heel spur can cause swelling at the front of the heel, along with inflammation and pain.
A heel spur stems from many of the same things that affect the plantar fascia. These include stress from repetitive movements like running, worn-out or poorly fitting shoes, and obesity. It also responds to many of the same treatments, such as rest, pain medications, or physical therapy.
On the other hand, the condition does show traits of a degenerative disease, including the abnormal structure of the collagen. Patients will also have thickened plantar fascia and calcified areas. The doctor will often find such changes through ultrasound.
Risk Factors
Certain risk factors increase the chances of developing an irritated plantar fascia. They include the following:
- Some types of exercise
- Age
- Obesity
- Certain occupations
- Foot mechanics
- High heels
Long-distance runners are particularly prone to inflammation of the plantar fascia. Generally speaking, activities that put a lot of stress on the heel and attached tissues increase the chances of developing an inflamed plantar fascia. Aerobic dancers and ballet dancers also have an increased risk.
Plantar fasciitis is most common in people who are between 40 and 60 years old.
Being overweight or obese increases the stress on the plantar fascia and thus increases the risk of inflammation. Pregnancy also puts more pressure on the plantar fascia.
Occupations that require people to stand for a long time, especially on hard surfaces, also increase the chances of developing inflammation of the plantar fascia. Examples include teachers and factory workers.
Specific problems with foot mechanics can put extra stress on the plantar fascia. People with high arches or flat feet, for example, have a higher chance of developing an irritated plantar fascia. Abnormal gaits can also stress the plantar fascia.
High heels, especially very high stiletto heels, cause a variety of foot problems. The shoes force the heel upward and thus shortens the Achilles tendon and other calf muscles. The shortened muscles and tendons put extra stress on the plantar fascia and can, therefore, damage it.
What Treatments Are Available?
The doctor will perform a physical exam and may order an imaging test like an X-ray or MRI to confirm the diagnosis. They want to make sure that the patient’s heel pain isn’t coming from something like a heel spur or fracture. After confirming that the patient does have an inflamed plantar fascia, the doctor will recommend a treatment plan. In 2001, the “American Family Physician” published a paper that described and critiqued the available treatments.
Home Remedies
In most cases, the doctor will start by advising the patient to treat their foot at home. They will suggest treatments like rest, braces, ice, and over-the-counter medications.
The doctor will also recommend various lifestyle changes, like losing excess weight or wearing shoes that provide excellent arch support, thick soles, and inserting extra cushioning. Women should not wear high heels, and patients of both sexes should replace worn-out athletic shoes. If the patient exercises, the doctor will recommend low-impact sports like bicycling or swimming instead of high-impact sports like jogging to put less stress on the feet.
Massaging one’s feet every night for 10 or 15 minutes can help ease chronic pain. It also provides a variety of other health benefits. For example, a foot massage can help strengthen ankle and foot muscles, especially if you also slowly rotate your foot. Stronger muscles will help prevent injuries like turned ankles.
Non-invasive Treatments
If home remedies and lifestyle changes don’t work, the next step is usually a corticosteroid injection. The doctor will typically administer the corticosteroid steroid in their office. They may use ultrasound to find the best place for the dose. Iontophoresis is a variation in which the doctor delivers a topical corticosteroid to the treatment area and then applies weak electrical currents to drive the medication deeper into the tissues.
The doctor may also recommend arch supports or night splints. An arch support is a type of orthotic that the patient wears inside the shoe. It distributes pressure across the foot and thus relieves the plantar fascia.
A night splint is a type of brace that the patient would wear during sleep. It keeps the foot flexed and lengthens both the Achilles tendon and the plantar fascia. A night splint can prevent the stiffness and pain that the patient usually experiences upon waking.
The doctor may suggest that the patient wear a boot cast, which looks like a ski boot, that would keep the foot immobile while the plantar fascia heals. The patient can take it off when they need to bathe.
Physical Therapy
Physical therapy is a standard treatment for plantar fasciitis. The physical therapist may work with the patient to help them improve their gait, strengthen the muscles of their lower legs, and otherwise put less pressure on the soles of their feet.
In many cases, the therapist will teach the patient a variety of stretching exercises that the patient will do twice or thrice a day. For example, the patient may stretch their calf muscles while standing with their hands against a wall.
In the “rolling stretch,” the patient will sit or stand and place a small ball or foam roller under their foot and move their foot back and forth for two minutes. The exercise will soon loosen tight muscles.
The patient can also stretch the plantar fascia itself by sitting down and crossing their foot across the other leg. The patient will then grip the toes and pull them back and hold them for about ten seconds. They can use the other hand to feel for tension in the plantar fascia. The patient should do exercises two or three times a day.
Surgery
Surgery is a last resort, only if the patient is in severe pain or has had plantar fasciitis for six to twelve months. The doctor will recommend surgery only if the patient has tried other and less invasive treatments with no results.
The surgeon may perform a plantar fascia release in which they detach the plantar fascia partway from the heel bone. While the procedure does relax the plantar fascia, it also makes the arch weaker.
The surgeon may recommend a procedure called a gastrocnemius recession if the patient still has a hard time flexing their feet even after physical therapy. In this procedure, the surgeon will make the calf muscle longer to lessen stress on the plantar fascia and increase ankle movement.
 Final Thoughts on Managing Your Plantar Fasciitis
Final Thoughts on Managing Your Plantar Fasciitis
While doctors can’t always determine the cause of plantar fasciitis, they can usually treat it. The vast majority of patients will need only the various non-invasive treatments like home remedies, physical therapy, or injections. Only the worst and most stubborn cases will need surgery.