Northwestern University scientists have created a new device that can shrink tumors rapidly by harnessing immune cells in tumor tissues. To do this, the team multiplied, sorted through, and harvested hundreds of millions of cells using a configurable microfluidic device. This method recovered 400% more of the tumor-eradicating cells than prior techniques.
Compared with other cancer therapies, the new approach tested in mice subjects could significantly shrink tumors. The findings were published on January 27, 2022, in the journal Nature Biomedical Engineering.
Currently, many cancer treatment therapies use dangerous chemicals and foreign substances that may cause unwanted side effects. Not to mention, these therapies tend to harm the body’s immune system, making patients more vulnerable to illnesses.
While immunotherapy – using the body’s cells and tissues to treat cancer – can shrink tumors in some cases, it’s not a foolproof method.
“People have been cured in the clinic of advanced melanoma through treatment with their own immune cells that were harvested out of tumor tissue,” said Shana O. Kelley, an expert in translational biotechnology and corresponding author on the paper. “The problem is, because of the way the cells are harvested, it only works in a very small number of patients.”
Kelley is a biochemistry and molecular genetics professor at Northwestern University Feinberg School of Medicine. She’s also the Neena B. Shwartz Professor of Chemistry and Biomedical Engineering at the Northwestern University Weinberg College of Arts and Sciences and McCormick School of Engineering.
Shortcomings of Current Cancer Treatments
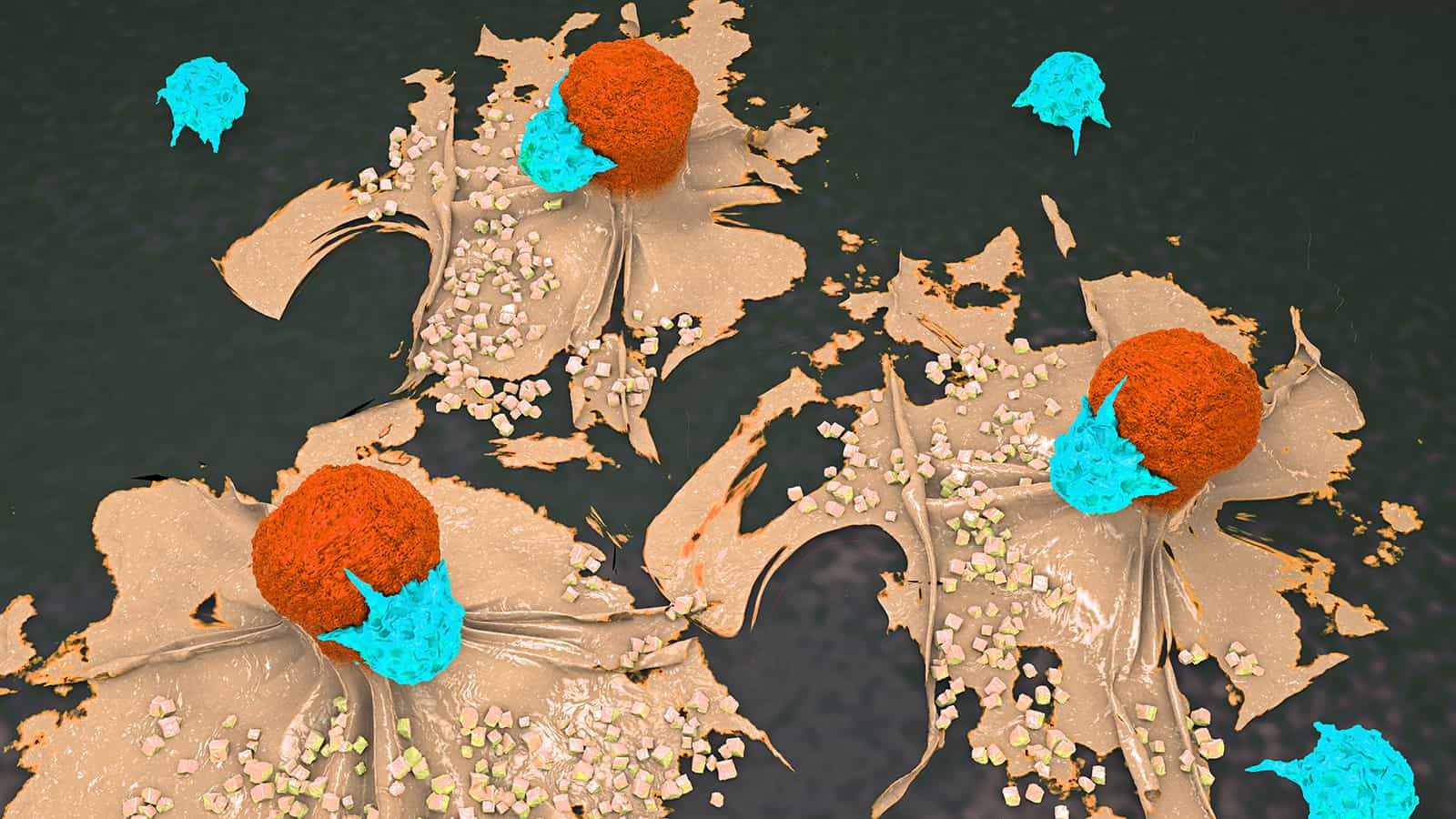
The targeted cells, called tumor-infiltrating lymphocytes (TILs), are potent, natural immune cells that penetrate tumor tissue. Researchers harvest these cells to shrink tumors; however, previous approaches haven’t always been successful.
In adoptive cell therapies used in clinics today, scientists use TILs with various phenotypes. This refers to the cells’ observable characteristics resulting from the interaction of their DNA with the environment. In many cases, scientists combine older and newer cells in cancer treatments. After they’ve extracted the TILs, they transport them to a lab to multiply and harvest them.
However, after they’ve populated and can return to the body, many cells have no energy left to fight the tumors. The cells have exhausted their resources after being in the body for so long.
Northwestern University Develops Method to Shrink Tumors
The team created a new technology to address this problem with current treatments. Researchers can identify the most active cells with microfluidic affinity targeting of infiltrating cells (MATIC). Using cell sorting techniques powered by nanotechnology, the scientists found the “Goldilocks population” of cells.
The scientists said this: “Compared with conventional cell sorting, immunomagnetic cell sorting recovered up to 30-fold higher numbers of TILs, and the higher levels and diversity of the recovered TILs accelerated TIL expansion and enhanced their therapeutic potency.
“Immunomagnetic cell sorting also allowed us to identify and isolate potent TIL subpopulations, in particular, TILs with moderate levels of CD39 (a marker of T-cell reactivity to tumours and T-cell exhaustion), which we found are tumour-specific, self-renewable and essential for the long-term success of adoptive cell therapies.”
By focusing on one cell phenotype, they noticed a significant shrinkage in tumors in the mice population. In fact, compared with traditional TIL cell therapies, the new method led to a dramatic uptick in survival rates. Also, the new technique could shrink tumors entirely in some cases.
“Instead of giving mice this mixture of cells with different phenotypes, we’re giving them the one cell phenotype that can actually help them,” Kelley said. “You see much more potency and a much higher response rate when you really home in on the sweet spot of T cell reactivity.”
The Future of the Cancer-Fighting Technology
The 3D-printed device offers another advantage that makes it feasible for hospital settings. The unimposing, easily replicated design means the technology doesn’t have to remain in laboratories. Having the cell therapy closer to patients would reduce costs and improve accessibility, benefiting more people.
Kelley joined Northwestern in August from the University of Toronto and continues researching how her device could improve cancer therapies. Currently, she’s using the technology to identify the same types of TILs in blood samples. This way, patients wouldn’t require surgery to remove small tumors before this type of cancer treatment.
She’s already launched a small company to make the technology commercially available. She also plans to collaborate with industry leaders and others at Northwestern to expand applications for the tool. So far, the platform has been utilized primarily for studying and measuring rare cells in the body.
“When we take on the development of a new technology, we typically end up with a hammer, and then need to go find a nail. We got introduced to problems in cell therapy, and it was immediately apparent that this was a perfect fit.” -Shana O. Kelley
The study’s first author, Ph.D. student Daniel Wang, also joined Northwestern from the University of Toronto as a postdoctoral fellow. He plans to keep improving cell therapies that shrink tumors in Kelley’s labs on the Chicago campus.
With this high-precision approach to treating cancer, hopefully, cancer rates will dramatically decline in the future. Sadly, cancer is a leading cause of death worldwide and accounted for nearly 10 million deaths in 2020, according to the WHO.
While cancer therapies play a pivotal role in treatment, you can reduce your cancer risk with lifestyle changes. Maintaining a healthy diet, exercising, reducing stress, avoiding tobacco and overindulgence in alcohol, and protecting yourself from UV radiation can help prevent cancer.
Final Thoughts on Scientists Finding a New Method to Shrink Tumors
As scientists continue to uncover new cancer treatments, it provides hope for millions worldwide. A team of scientists from Northwestern University developed a cutting-edge technology that improves the recovery of cancer-fighting cells. The device pinpoints the most active cells in tumors, which improves immunotherapy results. They’re currently working on making the devices commercially available for use in hospital settings.